Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
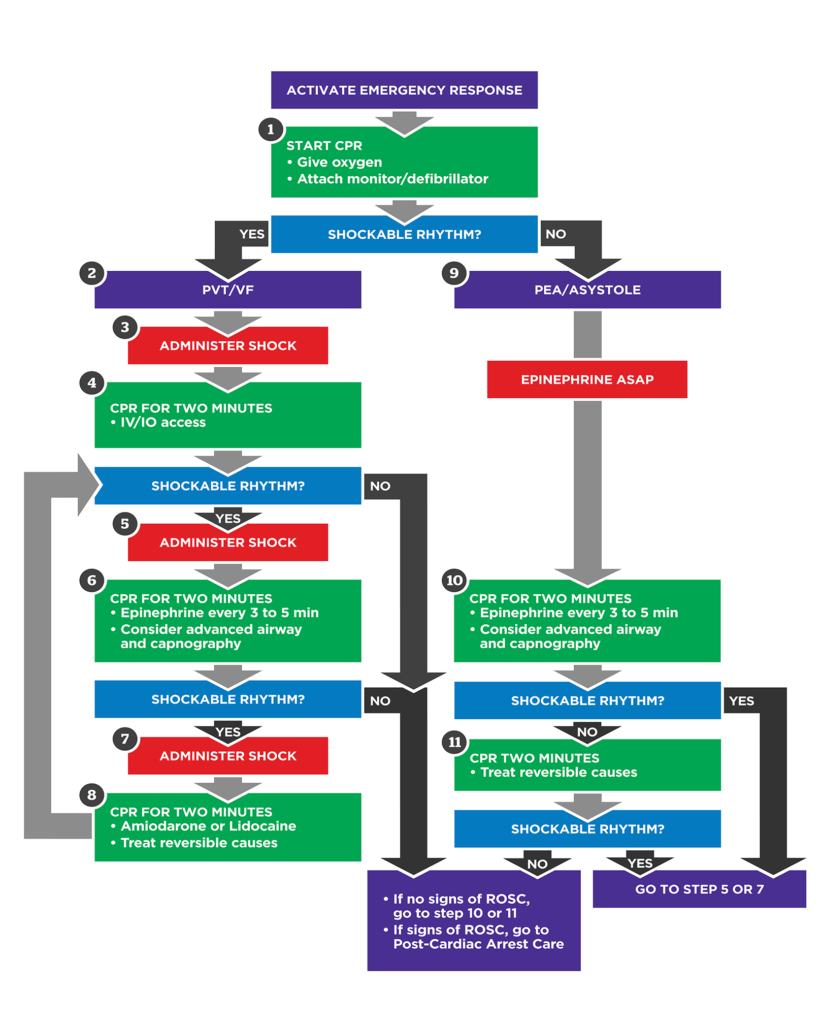
Advanced Cardiac Life Support ACLS Algorithms Drugs and Clinical Management Guide
Frequently Asked Questions
Advanced Cardiac Life Support ACLS is a set of evidence based clinical protocols used to manage adult cardiac arrest, peri arrest conditions, and life threatening cardiovascular emergencies using algorithms, medications, airway management, and team based resuscitation.
The primary goals of ACLS are early return of spontaneous circulation, optimization of oxygenation and perfusion, identification and treatment of reversible causes, prevention of neurological injury, and improvement of survival outcomes.
The shockable rhythms in ACLS are ventricular fibrillation and pulseless ventricular tachycardia. These rhythms require immediate defibrillation.
Asystole and pulseless electrical activity are non shockable rhythms and are managed with high quality CPR, epinephrine, and treatment of reversible causes.
Epinephrine is used in all cardiac arrest rhythms to increase coronary and cerebral perfusion pressure through vasoconstriction and is given every 3 to 5 minutes during resuscitation.
Amiodarone is indicated for shock refractory ventricular fibrillation or pulseless ventricular tachycardia after defibrillation attempts and epinephrine administration.
The Hs and Ts are reversible causes of cardiac arrest. Hs include hypoxia, hypovolemia, hydrogen ion excess acidosis, hypo or hyperkalemia, and hypothermia. Ts include tension pneumothorax, cardiac tamponade, toxins, coronary thrombosis, and pulmonary thrombosis.
High quality CPR includes a compression rate of 100 to 120 per minute, depth of 5 to 6 cm, full chest recoil, minimal interruptions, and avoidance of excessive ventilation.
Capnography is used to confirm advanced airway placement, monitor CPR quality, and detect return of spontaneous circulation. An end tidal CO2 less than 10 mmHg suggests poor CPR quality.
Symptomatic bradycardia is initially treated with atropine. If atropine is ineffective, transcutaneous pacing or infusion of dopamine or epinephrine is recommended.
Synchronized cardioversion is used for unstable tachyarrhythmias with a pulse, including unstable supraventricular tachycardia and unstable ventricular tachycardia.
Targeted temperature management involves maintaining body temperature between 32 and 36 degrees Celsius in comatose patients after return of spontaneous circulation to reduce neurological injury.
Post cardiac arrest care focuses on optimizing oxygenation, maintaining adequate blood pressure, treating the underlying cause, preventing secondary brain injury, and improving long term survival.
Termination of resuscitation may be considered when there is prolonged resuscitation with no return of spontaneous circulation, no identifiable reversible causes, persistently low end tidal CO2, and adherence to ACLS protocols.
Effective team communication using closed loop communication improves coordination, reduces errors, and enhances the efficiency and success of resuscitation efforts.