Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Addison’s Disease Comprehensive Clinical Guide Diagnosis Causes and Management
Frequently Asked Questions
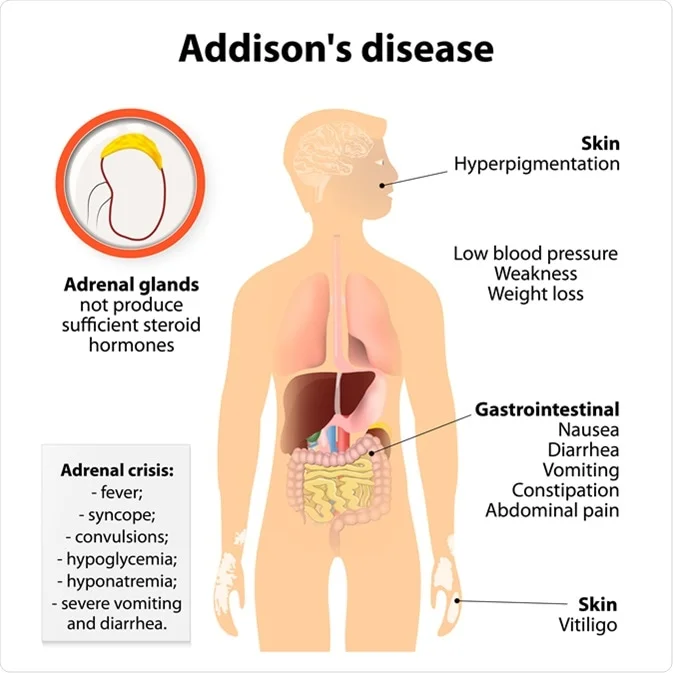
Addison’s disease is primary adrenal insufficiency caused by destruction or dysfunction of the adrenal cortex, resulting in deficiency of cortisol, aldosterone, and adrenal androgens.
Addison’s disease involves adrenal gland failure with high ACTH and hyperkalemia, while secondary adrenal insufficiency is due to pituitary or hypothalamic causes with normal aldosterone and no hyperkalemia.
Autoimmune adrenalitis is the most common cause in developed countries, while tuberculosis is the most common cause worldwide.
Loss of cortisol feedback causes elevated ACTH, which increases melanocyte-stimulating hormone activity, leading to hyperpigmentation.
Hyponatremia and hyperkalemia due to aldosterone deficiency are hallmark findings.
The ACTH (cosyntropin) stimulation test is the gold standard for diagnosis.
Addisonian crisis is a life-threatening emergency characterized by hypotension, shock, hypoglycemia, vomiting, and electrolyte imbalance.
Immediate IV hydrocortisone, aggressive IV normal saline with dextrose, correction of electrolytes, and treatment of the precipitating cause.
Lifelong glucocorticoid replacement with hydrocortisone and mineralocorticoid replacement with fludrocortisone.
During illness, surgery, or trauma, steroid requirements increase; failure to increase doses can precipitate adrenal crisis.
Addison’s disease cannot be cured, but it can be effectively managed with lifelong hormone replacement therapy.
Type 1 diabetes, autoimmune thyroid disease, pernicious anemia, and vitiligo as part of autoimmune polyglandular syndrome type 2.
Due to deficiency of adrenal androgens, which contribute to secondary sexual hair in women.
Never stopping steroids abruptly, carrying a medical alert ID, using stress dosing during illness, and having emergency injectable hydrocortisone.
With proper treatment, compliance, and patient education, the prognosis is excellent.