Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Blood Transfusion and Massive Blood Transfusion Protocol Complete Clinical Guide
Frequently Asked Questions
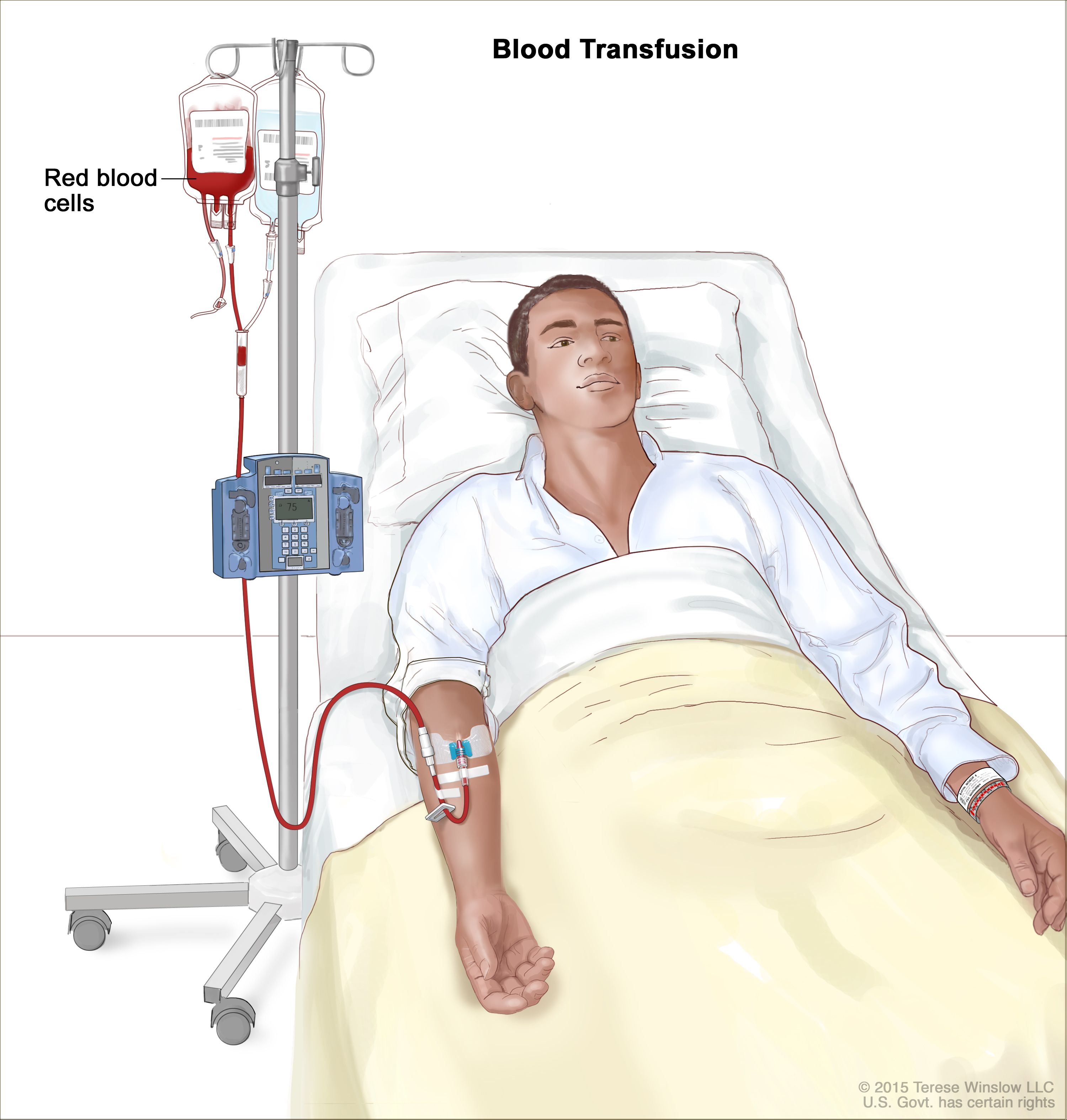
Blood transfusion is the intravenous administration of whole blood or specific blood components such as packed red blood cells, platelets, plasma, or cryoprecipitate to restore oxygen-carrying capacity, correct coagulopathy, or replace blood loss.
PRBC transfusion is indicated in acute blood loss, symptomatic anemia, hemoglobin less than 7 g/dL in stable adults, hemoglobin less than 8 g/dL in patients with cardiovascular disease, and ongoing hemorrhagic shock.
Massive blood transfusion is defined as transfusion of 10 or more units of PRBCs within 24 hours, 4 or more units within 1 hour with ongoing bleeding, or replacement of more than 50 percent of blood volume within 3 hours.
MTP should be activated in patients with life-threatening hemorrhage such as major trauma, postpartum hemorrhage, ruptured aneurysm, massive gastrointestinal bleeding, or uncontrolled surgical bleeding with hemodynamic instability.
The recommended ratio is 1:1:1 using packed red blood cells, fresh frozen plasma, and platelets to prevent dilutional coagulopathy and improve survival.
Citrate used as an anticoagulant in stored blood binds ionized calcium, leading to hypocalcemia which can cause hypotension, arrhythmias, and reduced myocardial contractility.
Common complications include febrile non-hemolytic transfusion reactions, allergic reactions, transfusion-associated circulatory overload, transfusion-related acute lung injury, hemolytic reactions, and transfusion-transmitted infections.
TRALI presents with acute hypoxemia, hypotension, and non-cardiogenic pulmonary edema, while TACO presents with hypertension, raised JVP, volume overload, elevated BNP, and improves with diuretics.
Monitoring includes hemoglobin, platelet count, INR, PT, aPTT, fibrinogen levels, arterial blood gas, lactate, ionized calcium, electrolytes, and core body temperature.
Tranexamic acid reduces fibrinolysis and mortality when given early within 3 hours of trauma-related hemorrhage, usually as a 1 g IV bolus followed by 1 g infusion over 8 hours.
Platelet transfusion is indicated when platelet count is below 10,000 per microliter prophylactically, below 20,000 with fever or sepsis, below 50,000 with active bleeding or surgery, and below 100,000 for neurosurgery.
FFP is indicated in active bleeding with INR greater than 1.5, massive transfusion, liver disease with bleeding, disseminated intravascular coagulation, and reversal of warfarin when PCC is unavailable.
Cryoprecipitate is rich in fibrinogen, factor VIII, factor XIII, and von Willebrand factor, and is used when fibrinogen levels fall below 150 to 200 mg/dL, especially in massive hemorrhage or DIC.
The first step is to immediately stop the transfusion, maintain intravenous access with normal saline, assess the patient, and send blood and urine samples for hemolysis workup.
MTP should be discontinued once bleeding is controlled, the patient is hemodynamically stable, transfusion requirements decrease, and coagulation parameters begin to normalize.