Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
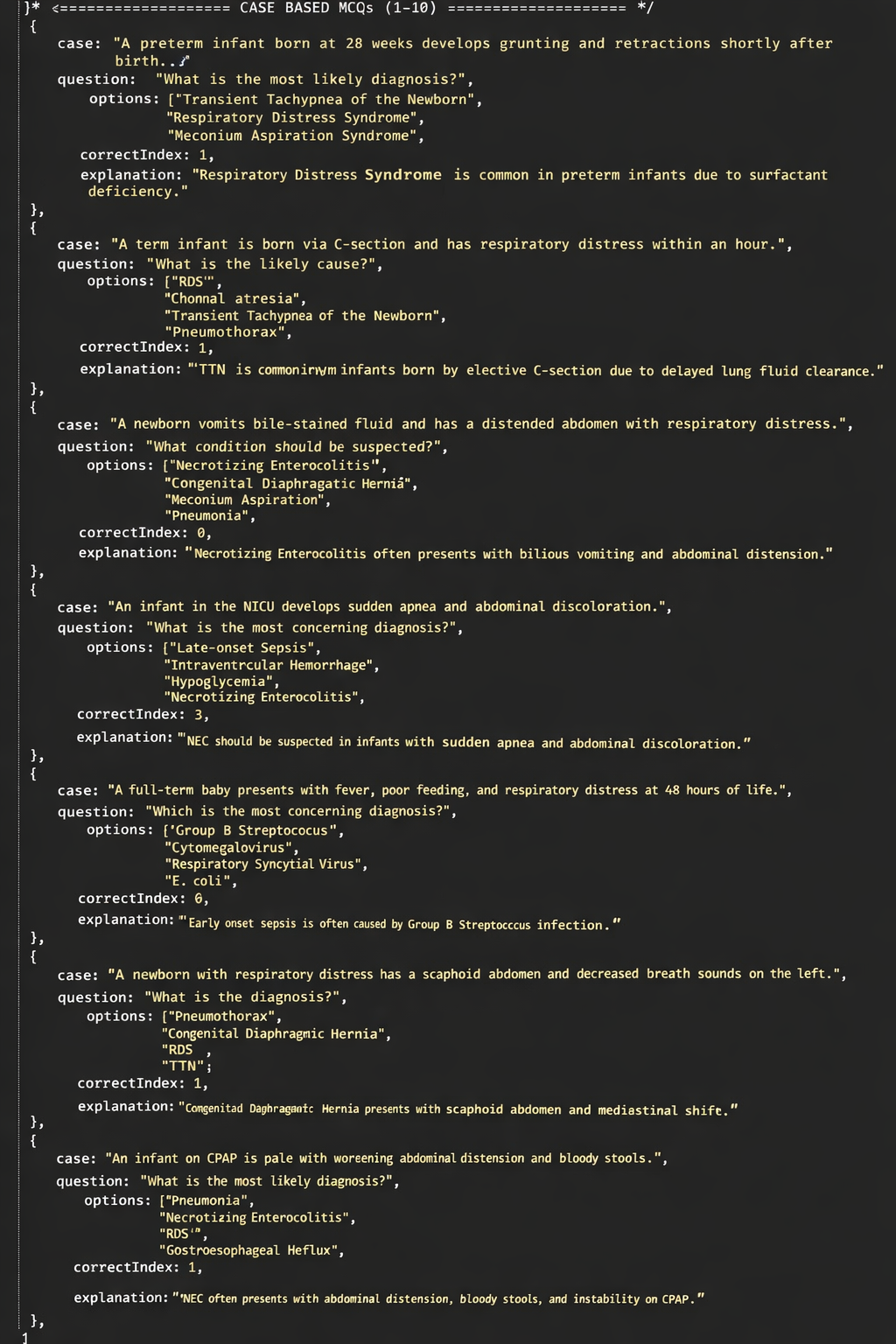
Respiratory Distress in Newborn Causes, Signs, Diagnosis and Management
Frequently Asked Questions
Respiratory distress in a newborn is a condition where the baby has difficulty breathing, usually within the first hours or days after birth. It is characterized by tachypnea, chest retractions, nasal flaring, grunting, and sometimes cyanosis.
Common signs include respiratory rate above 60 breaths per minute, nasal flaring, chest wall retractions, expiratory grunting, cyanosis, poor feeding, apnea, and increased work of breathing.
The most common cause is Respiratory Distress Syndrome (RDS), which occurs due to surfactant deficiency leading to alveolar collapse and impaired gas exchange.
TTN is a mild respiratory condition caused by delayed clearance of fetal lung fluid. It is common in term infants delivered by cesarean section and usually resolves within 24–72 hours.
Meconium aspiration occurs when a stressed fetus inhales meconium-stained amniotic fluid, leading to airway obstruction, chemical pneumonitis, infection risk, and persistent pulmonary hypertension.
PPHN is a condition where pulmonary vascular resistance remains high after birth, causing right-to-left shunting and severe hypoxemia. It is often associated with MAS, sepsis, or birth asphyxia.
Yes. Early-onset neonatal sepsis commonly presents with respiratory distress, poor feeding, lethargy, temperature instability, apnea, and signs of shock. Group B Streptococcus and E. coli are common pathogens.
Congenital causes include congenital diaphragmatic hernia, choanal atresia, tracheoesophageal fistula, Pierre Robin sequence, and congenital heart diseases like transposition of great arteries.
Diagnosis is based on clinical examination and investigations such as pulse oximetry, arterial blood gas analysis, chest X-ray, blood cultures, CBC, CRP, and echocardiography when cardiac causes are suspected.
Initial management includes maintaining airway and breathing, providing supplemental oxygen, CPAP or mechanical ventilation if required, treating underlying causes such as surfactant for RDS, antibiotics for infection, or surgery for congenital defects.
RDS occurs mainly in preterm infants due to surfactant deficiency and worsens without treatment. TTN occurs in term infants due to delayed lung fluid clearance and usually resolves within a few days.
Surfactant therapy is indicated in premature infants with Respiratory Distress Syndrome to reduce alveolar surface tension, improve lung compliance, and enhance oxygenation.
Untreated respiratory distress can lead to hypoxemia, acidosis, pulmonary hypertension, air leak syndromes, multi-organ dysfunction, and increased neonatal mortality.
Inhaled nitric oxide is used in severe cases of PPHN to selectively dilate pulmonary vessels, reduce pulmonary artery pressure, and improve oxygenation.
Emergency causes include pneumothorax, pulmonary hemorrhage, severe sepsis with shock, critical congenital heart disease, and airway obstruction.