Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Neonatal Hypothermia and Hypoglycemia Diagnosis Causes Management Guide
Frequently Asked Questions
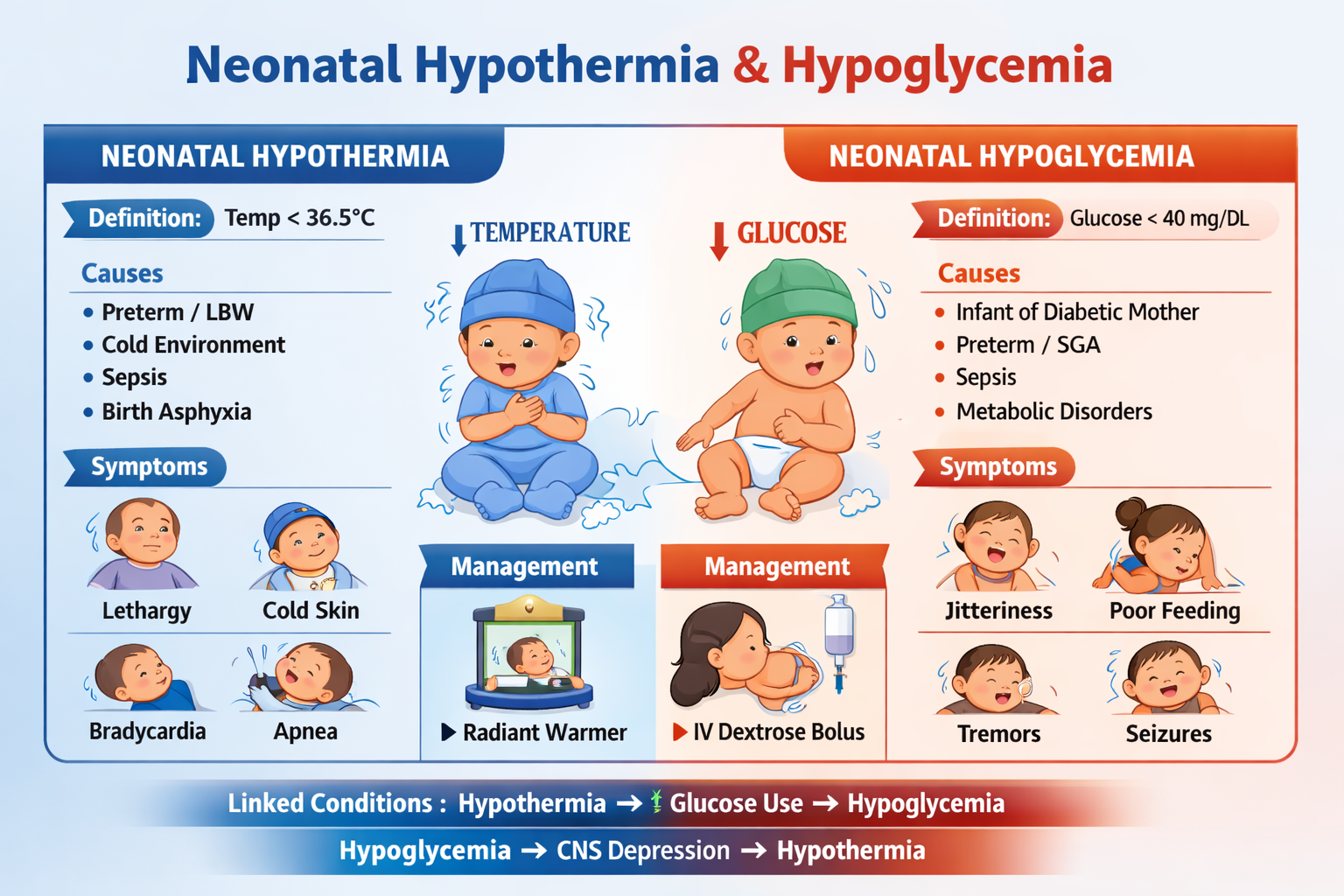
Neonatal hypothermia is defined as a newborn core body temperature below 36.5°C. It occurs because neonates have immature thermoregulation, large surface area, thin skin, and limited fat stores.
WHO classifies neonatal hypothermia as mild (36.0–36.4°C), moderate (32.0–35.9°C), and severe (<32°C).
Newborns lose heat rapidly due to large surface area-to-weight ratio, minimal subcutaneous fat, inability to shiver effectively, and reliance on brown fat metabolism for heat production.
Major causes include cold delivery environments, delayed drying and wrapping, prematurity, low birth weight, neonatal sepsis, birth asphyxia, and inadequate warming during transport.
Signs include cold skin, lethargy, poor feeding, tachypnea, bradycardia, apnea, metabolic acidosis, hypoglycemia, and increased risk of sepsis.
Neonatal hypoglycemia refers to low blood glucose levels in newborns, commonly defined as <45 mg/dL after 24 hours of life, which can cause neuroglycopenia and seizures if untreated.
High-risk groups include infants of diabetic mothers, preterm babies, small for gestational age infants, large for gestational age infants, babies with sepsis, hypothermia, or birth asphyxia.
Symptoms include jitteriness, tremors, poor feeding, lethargy, apnea, hypotonia, cyanosis, and seizures in severe or prolonged cases.
Hypothermia increases glucose consumption due to cold stress, leading to hypoglycemia. Hypoglycemia causes CNS depression, reducing thermoregulation and worsening hypothermia.
Symptomatic or severe hypoglycemia is treated immediately with 10% dextrose bolus 2 mL/kg IV, followed by continuous glucose infusion with close monitoring.
Management includes immediate drying, skin-to-skin warming for mild cases, radiant warmer or incubator care for moderate cases, controlled rewarming in NICU for severe cases, and treating underlying causes like sepsis.
Untreated hypothermia can cause hypoglycemia, metabolic acidosis, respiratory failure, persistent pulmonary hypertension, shock, and increased neonatal mortality.
Untreated hypoglycemia can lead to seizures, permanent brain injury, developmental delay, cerebral palsy, and increased risk of death.
Key investigations include plasma glucose confirmation, insulin levels, ketones, cortisol, growth hormone, metabolic screening, and evaluation for congenital hyperinsulinism or endocrine disorders.
Prevention includes maintaining the warm chain at birth, early drying and wrapping, kangaroo mother care, early breastfeeding, screening high-risk newborns, and ensuring proper NICU thermal support.