Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Osteomyelitis Causes Symptoms Diagnosis Treatment and Prevention Guide
Frequently Asked Questions
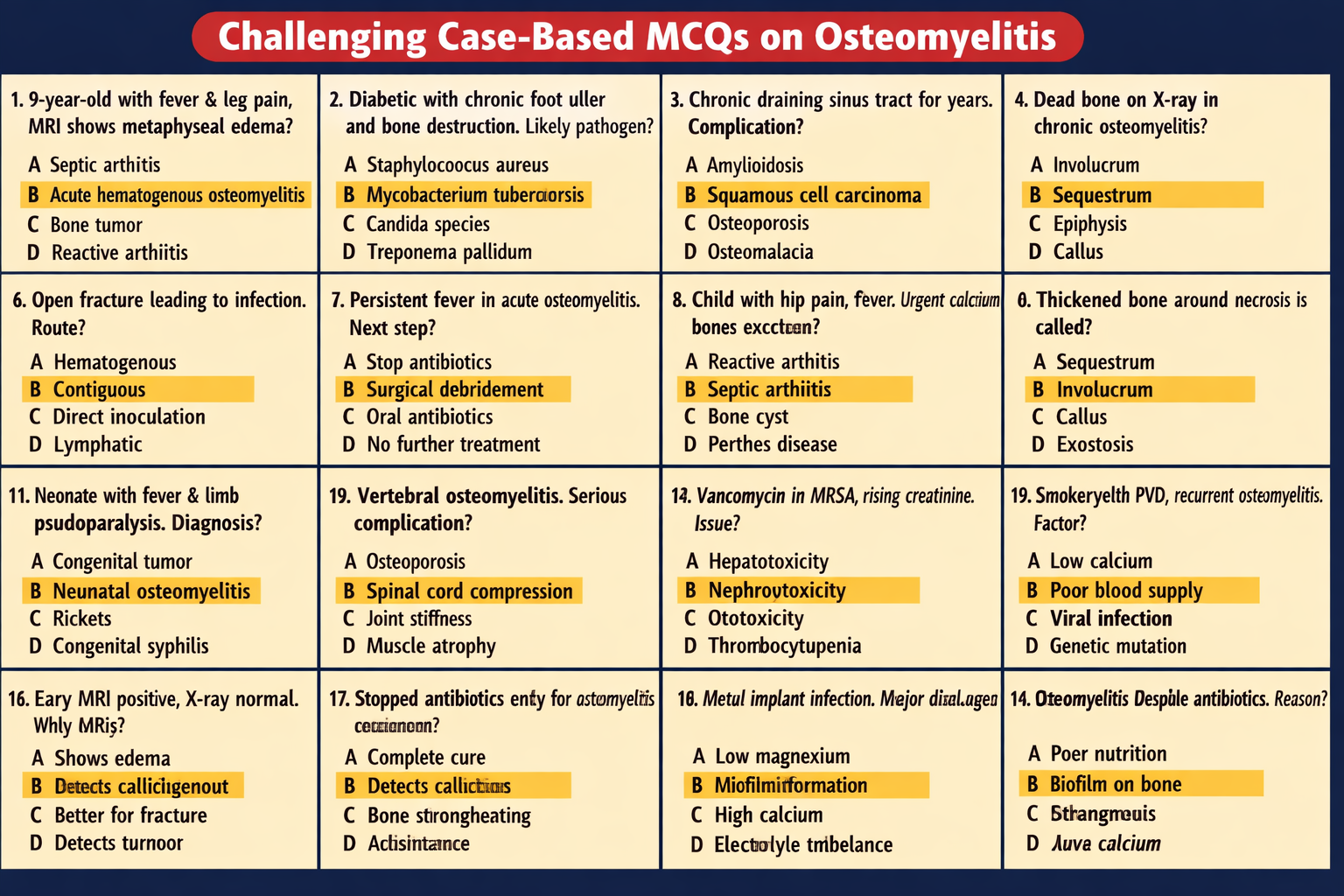
Osteomyelitis is a serious infection of bone caused by bacteria or fungi, leading to inflammation, bone destruction, and possible chronic complications if untreated.
It is commonly caused by bacteria such as Staphylococcus aureus. Infection can spread through the bloodstream, from nearby tissues, or through direct contamination after trauma or surgery.
Symptoms include bone pain, swelling, warmth, redness, fever, fatigue, difficulty moving the affected limb, and sometimes pus discharge in chronic cases.
Acute osteomyelitis develops rapidly over days to weeks, while chronic osteomyelitis persists for months or years with recurring infections and dead bone formation.
High-risk groups include diabetics, immunocompromised individuals, IV drug users, trauma patients, elderly individuals, and those with poor circulation or chronic wounds.
Diagnosis involves blood tests, ESR and CRP levels, imaging such as MRI or X-ray, blood cultures, and confirmation with bone biopsy and culture.
MRI can detect early bone marrow edema and inflammation before changes appear on X-rays, making it the most sensitive early diagnostic tool.
The most common organism is Staphylococcus aureus. Others include MRSA, Streptococcus, Salmonella in sickle cell disease, Pseudomonas, and fungal pathogens in immunocompromised patients.
A sequestrum is a piece of dead bone separated from healthy bone due to infection and lack of blood supply.
An involucrum is new bone that forms around dead bone as a reactive protective response in chronic osteomyelitis.
Treatment includes prolonged IV antibiotics, pain management, immobilization, and surgical debridement if there is abscess or necrotic bone.
Acute cases typically require 4–6 weeks of antibiotics, while chronic cases may need 6–12 weeks or longer depending on severity.
Surgery is required when there is dead bone, abscess formation, persistent infection despite antibiotics, or implant-associated infection.
Complications include chronic infection, bone deformity, pathological fractures, growth disturbances in children, sepsis, amputation, and rare malignant transformation.
Yes, recurrence is possible, especially if antibiotics are stopped early or if necrotic bone remains.
Diabetes causes poor circulation, neuropathy, and chronic ulcers, which allow infection to spread into bone.
Vertebral osteomyelitis is infection of spinal bones, which can cause back pain, fever, and potentially dangerous spinal cord compression.
Prevention includes proper wound care, early infection treatment, diabetic foot care, sterile surgical practices, and maintaining good immunity and nutrition.
If untreated, it can lead to sepsis, severe disability, or death, but early diagnosis and treatment greatly improve outcomes.
Patients should complete antibiotic courses, control blood sugar, avoid smoking, maintain nutrition, attend follow-ups, and perform rehabilitation exercises.