Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
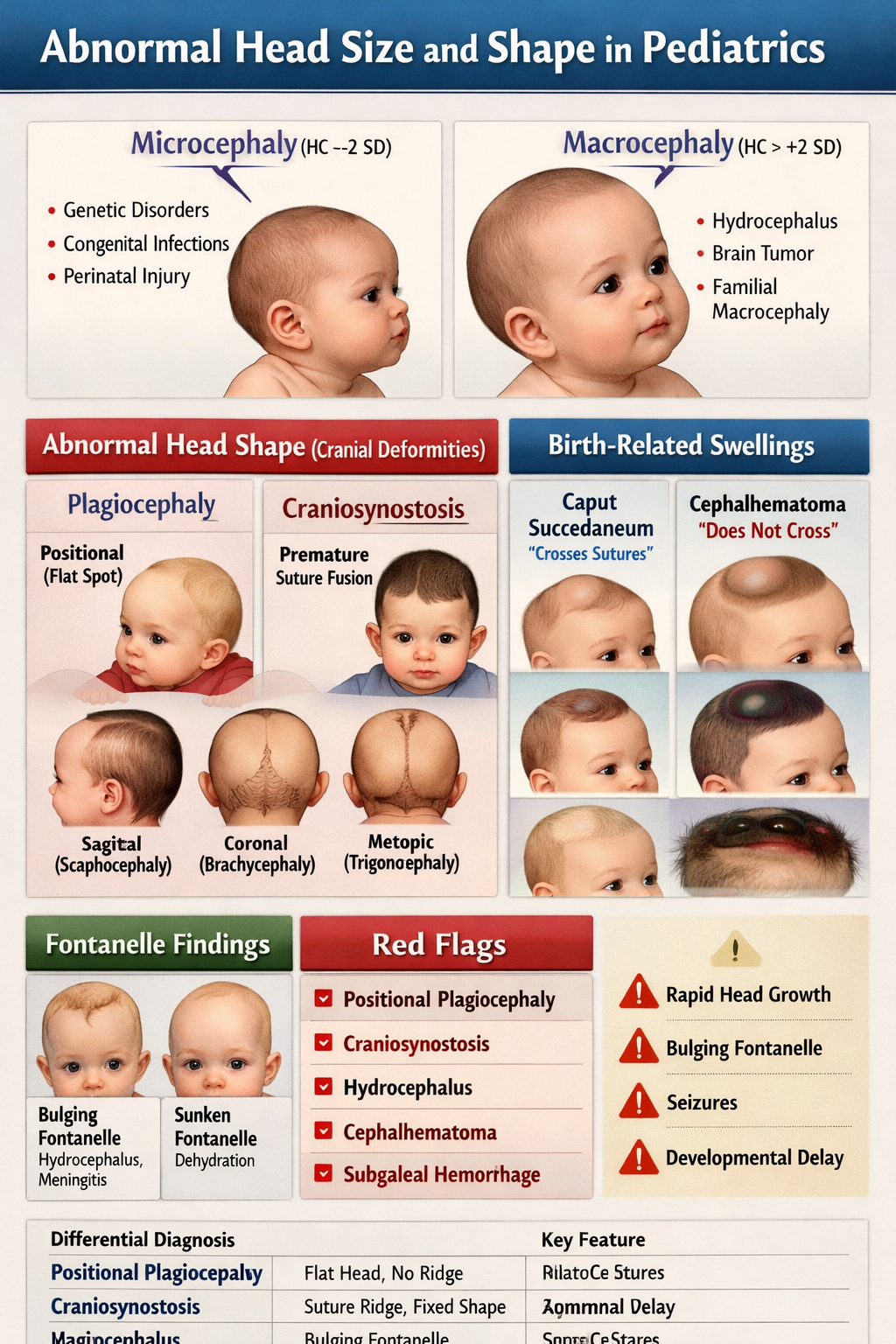
Abnormal Head Size and Shape in Pediatrics Microcephaly Macrocephaly Craniosynostosis Guide
Frequently Asked Questions
Head circumference is abnormal when it falls below –2 standard deviations (microcephaly) or above +2 standard deviations (macrocephaly) for age and sex on standardized growth charts.
Microcephaly is defined as a head circumference less than –2 SD below the mean, indicating reduced brain growth and often associated with developmental delay or neurologic impairment.
Common causes include congenital infections (CMV, Zika), chromosomal abnormalities, genetic syndromes, perinatal hypoxic injury, severe malnutrition, and metabolic disorders.
Macrocephaly is defined as head circumference greater than +2 SD above the mean. It may be benign familial or due to serious intracranial pathology such as hydrocephalus.
Causes include benign familial macrocephaly, benign enlargement of subarachnoid spaces (BESS), hydrocephalus, intracranial tumors, subdural hematoma, and storage disorders like Tay-Sachs.
Benign macrocephaly usually has normal development and stable growth, while hydrocephalus presents with rapid head enlargement, bulging fontanelle, vomiting, sunset eye sign, and raised intracranial pressure.
Plagiocephaly refers to asymmetrical flattening of the skull, most commonly positional due to prolonged supine positioning, and is usually benign.
Positional plagiocephaly has no suture ridging and improves with repositioning, whereas craniosynostosis involves premature suture fusion, palpable ridging, fixed deformity, and may cause raised intracranial pressure.
Craniosynostosis is the premature fusion of one or more cranial sutures, leading to abnormal head shape and potential restriction of brain growth.
Sagittal fusion causes scaphocephaly, coronal fusion causes brachycephaly or anterior plagiocephaly, metopic fusion causes trigonocephaly, and lambdoid fusion causes posterior plagiocephaly.
CT scan with 3D reconstruction is the gold standard investigation for confirming craniosynostosis and identifying the fused suture.
Caput succedaneum is scalp edema present at birth that crosses suture lines and resolves spontaneously within 1–2 days.
Cephalhematoma is a subperiosteal hemorrhage that does not cross suture lines, appears hours after birth, and may lead to neonatal jaundice.
Subgaleal hemorrhage is bleeding into the subaponeurotic space, often after vacuum delivery. It can cause massive blood loss, shock, and is a neonatal emergency.
Red flags include rapidly increasing head circumference, bulging fontanelle, seizures, vomiting, developmental regression, suspected craniosynostosis, signs of raised intracranial pressure, or suspected abusive head trauma.