Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
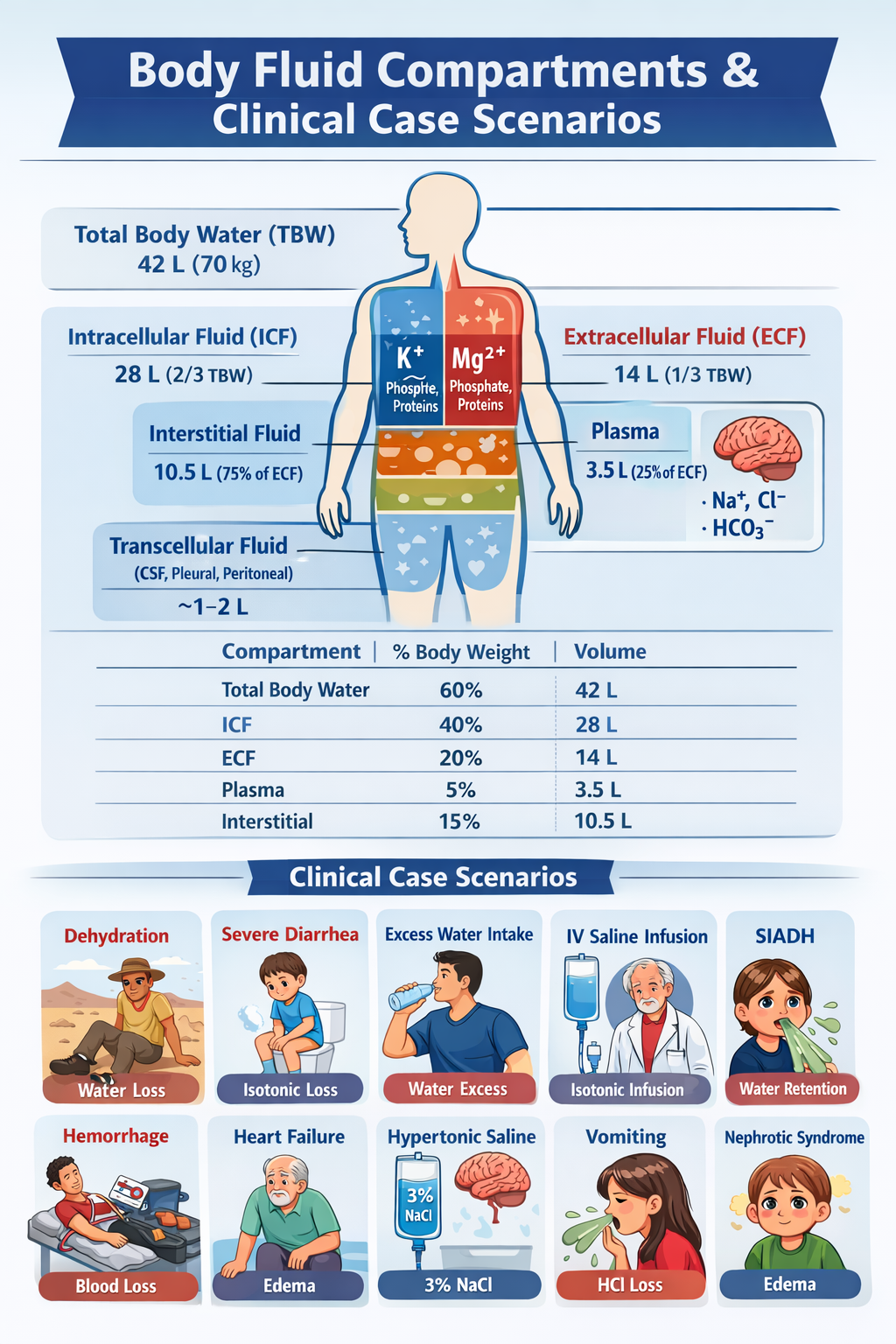
Body Fluid Compartments Explained with Clinical Case Scenarios and Fluid Shifts
Frequently Asked Questions
Body fluid compartments are the different spaces in the body where water is distributed, mainly divided into intracellular fluid (ICF) and extracellular fluid (ECF).
Total body water is the total amount of water in the human body, approximately 60% of body weight in adult males and 50% in adult females.
TBW is distributed as two-thirds inside cells (ICF) and one-third outside cells (ECF).
Intracellular fluid is the fluid contained within body cells and makes up about 40% of body weight or 28 liters in a 70 kg adult male.
Extracellular fluid is the fluid outside body cells and makes up about 20% of body weight or 14 liters in a 70 kg adult male.
ECF is subdivided into interstitial fluid (75% of ECF), plasma (25% of ECF), and a small transcellular fluid component.
Interstitial fluid is the fluid present between tissue cells, accounting for about 10.5 liters in a 70 kg adult male.
Plasma volume is the fluid component of blood inside vessels, accounting for about 3.5 liters in a 70 kg adult male.
Transcellular fluid is a specialized part of ECF found in spaces such as cerebrospinal fluid, pleural fluid, peritoneal fluid, and synovial fluid.
Potassium (K+), magnesium (Mg2+), phosphate, and proteins are the dominant intracellular ions.
Sodium (Na+), chloride (Cl−), and bicarbonate (HCO3−) are the dominant extracellular ions.
ECF osmolarity increases, causing water to shift from ICF to ECF, leading to contraction of both compartments (hyperosmotic volume contraction).
Diarrhea causes isotonic fluid loss mainly from the ECF, producing isosmotic volume contraction with no major ICF change.
Excess water decreases plasma osmolarity, causing water movement into cells, expanding both ICF and ECF (hyposmotic volume expansion).
0.9% normal saline is isotonic, so it stays within the extracellular compartment and expands plasma and interstitial volumes.
Hypertonic saline increases ECF osmolarity, pulling water out of cells, expanding ECF and shrinking ICF.
SIADH causes excess water retention, leading to hyposmotic volume expansion with both ECF and ICF expansion.
Loss of albumin reduces plasma oncotic pressure, causing fluid shift from plasma into interstitial space, producing edema.
Heart failure increases venous and capillary hydrostatic pressure, pushing fluid into interstitial space and expanding ECF volume.
Rapid correction can cause osmotic demyelination syndrome (central pontine myelinolysis), leading to severe neurological damage.