Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
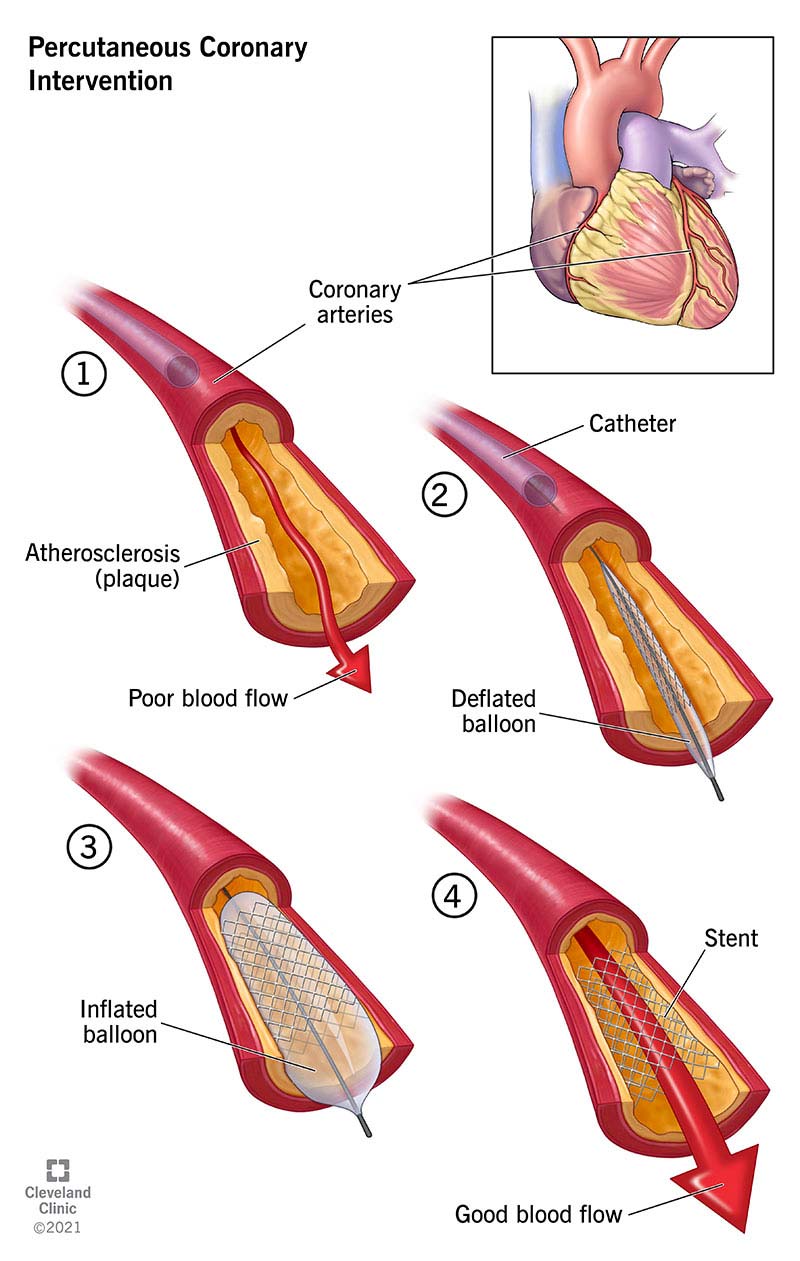
Percutaneous Coronary Intervention PCI Procedure Indications Steps Complications Management
Frequently Asked Questions
Percutaneous Coronary Intervention is a minimally invasive catheter-based procedure used to restore blood flow in narrowed or occluded coronary arteries, usually by balloon angioplasty followed by stent implantation.
PCI is indicated in ST-elevation myocardial infarction (primary PCI), high-risk NSTEMI or unstable angina, chronic stable angina with significant ischemia, and selected cases of left main or proximal LAD disease.
Primary PCI refers to immediate PCI performed as the first reperfusion strategy in acute STEMI, ideally within 90–120 minutes of first medical contact.
Coronary angioplasty refers only to balloon dilatation of a coronary artery, whereas PCI includes angioplasty plus stent implantation and adjunctive pharmacotherapy.
Drug-eluting stents are coronary stents coated with antiproliferative drugs that inhibit neointimal hyperplasia, thereby reducing the risk of in-stent restenosis.
Drug-eluting stents significantly reduce restenosis rates compared to bare-metal stents, making them the standard of care in most PCI procedures.
Dual antiplatelet therapy consists of aspirin plus a P2Y12 inhibitor (clopidogrel, prasugrel, or ticagrelor) to prevent stent thrombosis after PCI.
After PCI with drug-eluting stents, DAPT is recommended for at least 12 months in acute coronary syndrome and at least 6 months in stable coronary artery disease, unless bleeding risk is high.
The common access routes for PCI are the radial artery and femoral artery, with radial access preferred due to lower bleeding complications.
No-reflow is a complication where there is inadequate myocardial perfusion despite successful opening of the epicardial coronary artery, usually due to microvascular obstruction.
Major complications include stent thrombosis, coronary dissection or perforation, no-reflow phenomenon, contrast-induced nephropathy, bleeding, and vascular access complications.
Contrast-induced nephropathy is acute kidney injury occurring after exposure to contrast media during PCI, characterized by a rise in serum creatinine within 48–72 hours.
CABG is preferred in patients with diabetes and multivessel disease, left main disease with high SYNTAX score, and complex coronary anatomy unsuitable for PCI.
In-stent restenosis is re-narrowing of a stented coronary segment due to neointimal hyperplasia, typically occurring months after PCI.
Late stent thrombosis is the most feared late complication of PCI because it can lead to sudden myocardial infarction and death.