Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
Diseases of the Pericardium Clinical Guide Acute Pericarditis Cardiac Tamponade
Frequently Asked Questions
The major diseases of the pericardium include acute pericarditis, pericardial effusion, cardiac tamponade, and constrictive pericarditis. These conditions vary from inflammatory to life-threatening hemodynamic disorders.
Acute pericarditis typically presents with sharp pleuritic chest pain that improves on sitting forward, fever, pericardial friction rub, and characteristic ECG changes such as diffuse ST elevation with PR depression.
Diagnosis requires at least two of the following: typical chest pain, pericardial friction rub, characteristic ECG changes, or new or worsening pericardial effusion. Elevated inflammatory markers support the diagnosis.
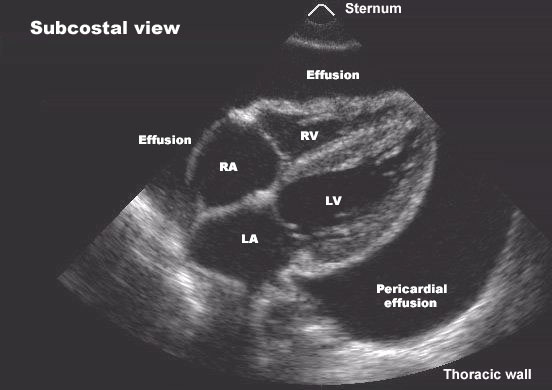
Pericardial effusion can be caused by pericarditis, malignancy, tuberculosis, uremia, hypothyroidism, trauma, autoimmune diseases, or post-cardiac surgery.
Pericardial effusion progresses to cardiac tamponade when intrapericardial pressure rises enough to impair cardiac filling, leading to hypotension, elevated jugular venous pressure, and reduced cardiac output.
Key signs include hypotension, elevated jugular venous pressure, tachycardia, muffled heart sounds, and pulsus paradoxus. Echocardiography confirms the diagnosis.
The definitive treatment of cardiac tamponade is urgent pericardiocentesis to relieve pressure on the heart. Supportive measures are only temporary and should not delay drainage.
Constrictive pericarditis is a chronic condition caused by fibrotic or calcified pericardium that restricts diastolic filling of the heart, leading to symptoms of right-sided heart failure.
Constrictive pericarditis shows marked ventricular interdependence, respiratory variation in ventricular filling, pericardial thickening or calcification, and may demonstrate a pericardial knock, unlike restrictive cardiomyopathy.
Pericardiectomy is the definitive treatment for symptomatic chronic constrictive pericarditis. Diuretics may provide temporary symptom relief but are not curative.