Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
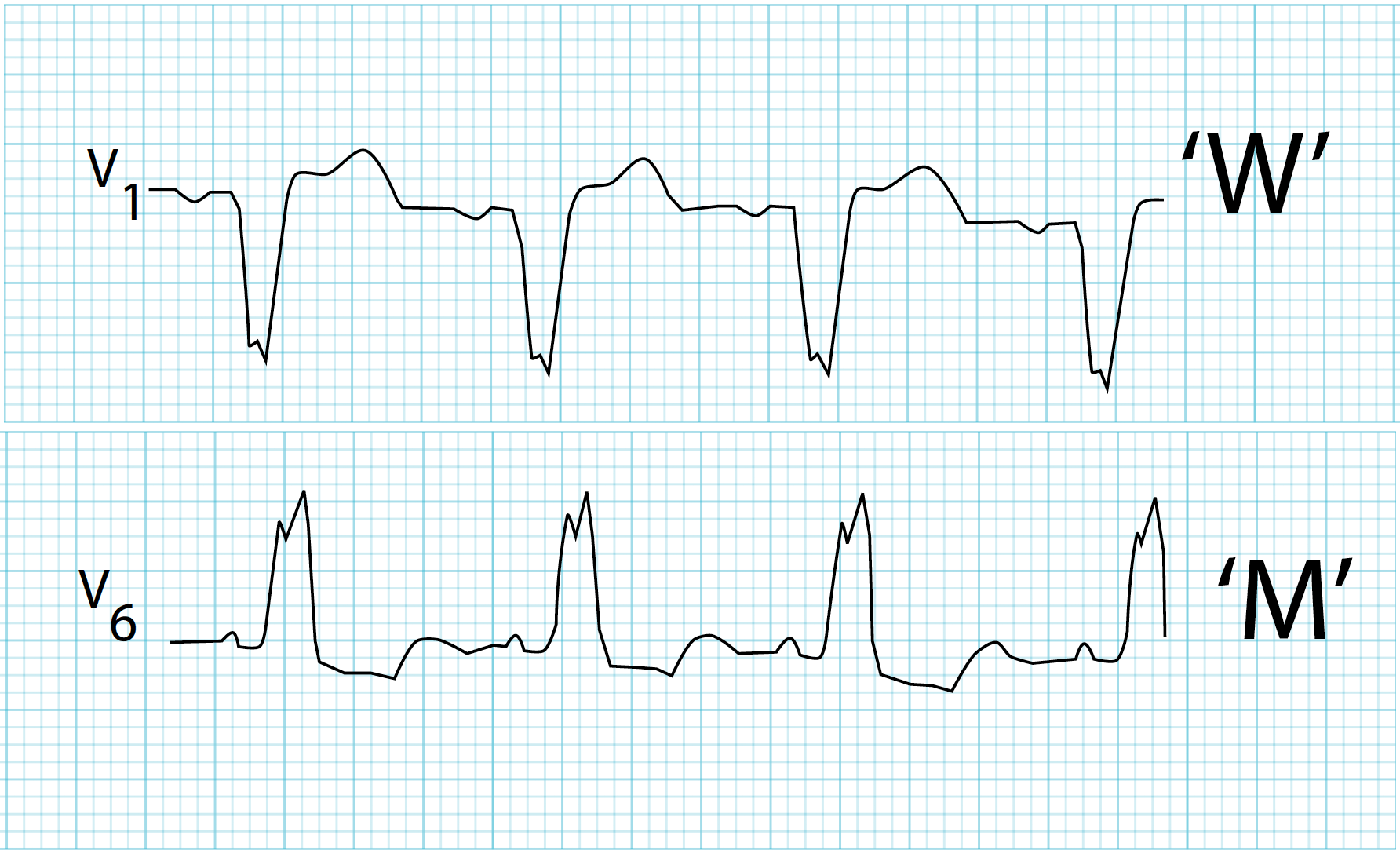
Bundle Branch Block Clinical Features Diagnosis and Management Guide
Frequently Asked Questions
A bundle branch block is a cardiac conduction abnormality in which electrical impulses are delayed or blocked in the right or left bundle branch of the His–Purkinje system, resulting in widened QRS complexes and asynchronous ventricular depolarization on ECG.
Right bundle branch block affects right ventricular depolarization and is often benign, while left bundle branch block affects left ventricular depolarization and is usually associated with underlying structural heart disease and worse prognosis.
Common causes include hypertension with left ventricular hypertrophy, ischemic heart disease, cardiomyopathy, aortic stenosis, myocardial infarction, and degenerative conduction system disease.
No, many patients with bundle branch block are asymptomatic. Symptoms such as syncope, dizziness, or dyspnea usually indicate associated heart disease or progression to advanced conduction block.
New-onset left bundle branch block can mask ischemic ECG changes and is treated as a STEMI equivalent because it often represents acute myocardial infarction requiring urgent reperfusion.
Diagnosis is made using a 12-lead ECG showing QRS duration of 120 ms or more with characteristic morphologic patterns specific to right or left bundle branch block.
Isolated asymptomatic right bundle branch block usually does not require treatment. Management focuses on identifying and treating any underlying cardiac or pulmonary condition.
A pacemaker is indicated in patients with bundle branch block who develop symptomatic high-grade atrioventricular block, recurrent syncope due to conduction disease, alternating bundle branch block, or trifascicular disease.
Cardiac resynchronization therapy is recommended in patients with heart failure, reduced ejection fraction (≤35%), left bundle branch block morphology, and wide QRS duration to improve symptoms and survival.
Prognosis depends on the type and underlying cause. Isolated right bundle branch block has a good prognosis, while left bundle branch block is associated with increased risk of heart failure, arrhythmias, and cardiovascular mortality.