Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
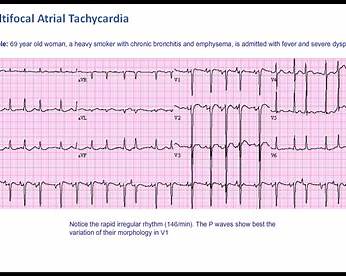
Multifocal Atrial Tachycardia Clinical Features ECG Diagnosis and Management
Frequently Asked Questions
Multifocal atrial tachycardia is a supraventricular tachyarrhythmia characterized by an irregular rhythm, heart rate greater than 100 beats per minute, and at least three different P-wave morphologies on ECG, caused by multiple ectopic atrial pacemakers.
The most common cause of multifocal atrial tachycardia is hypoxia, most frequently seen in patients with chronic obstructive pulmonary disease or acute pulmonary illnesses.
MAT is diagnosed on ECG by the presence of an irregularly irregular rhythm, heart rate over 100 per minute, at least three distinct P-wave morphologies, variable PR intervals, and an isoelectric baseline between P waves.
MAT shows discrete P waves with different morphologies and an isoelectric baseline, whereas atrial fibrillation has no distinct P waves and shows continuous fibrillatory activity.
Wandering atrial pacemaker has similar ECG features to MAT but the heart rate is less than 100 beats per minute, whereas MAT has a heart rate greater than 100 beats per minute.
The most important step is treatment of the underlying cause, such as correcting hypoxia, treating pulmonary disease, managing infection, and correcting electrolyte abnormalities.
Magnesium sulfate and non-dihydropyridine calcium channel blockers such as verapamil or diltiazem are preferred for rate control in MAT.
Beta blockers are generally avoided or used cautiously because many MAT patients have underlying COPD or asthma, where beta blockers may worsen bronchospasm.
No, electrical cardioversion is ineffective in MAT because the arrhythmia is due to enhanced automaticity rather than a re-entrant mechanism.
No, anticoagulation is not indicated in multifocal atrial tachycardia as it does not increase the risk of thromboembolism.
Hypokalemia and hypomagnesemia are commonly associated with MAT and should be corrected promptly.
No, digoxin is generally ineffective in MAT and may worsen the arrhythmia due to increased atrial automaticity.
Drugs such as theophylline, beta-agonists, and excess catecholamines can precipitate or worsen MAT.
The prognosis depends on the severity of the underlying illness; MAT itself is usually benign but is often a marker of severe systemic or pulmonary disease.
MAT is most commonly seen in elderly patients with severe pulmonary disease, particularly chronic obstructive pulmonary disease.