Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
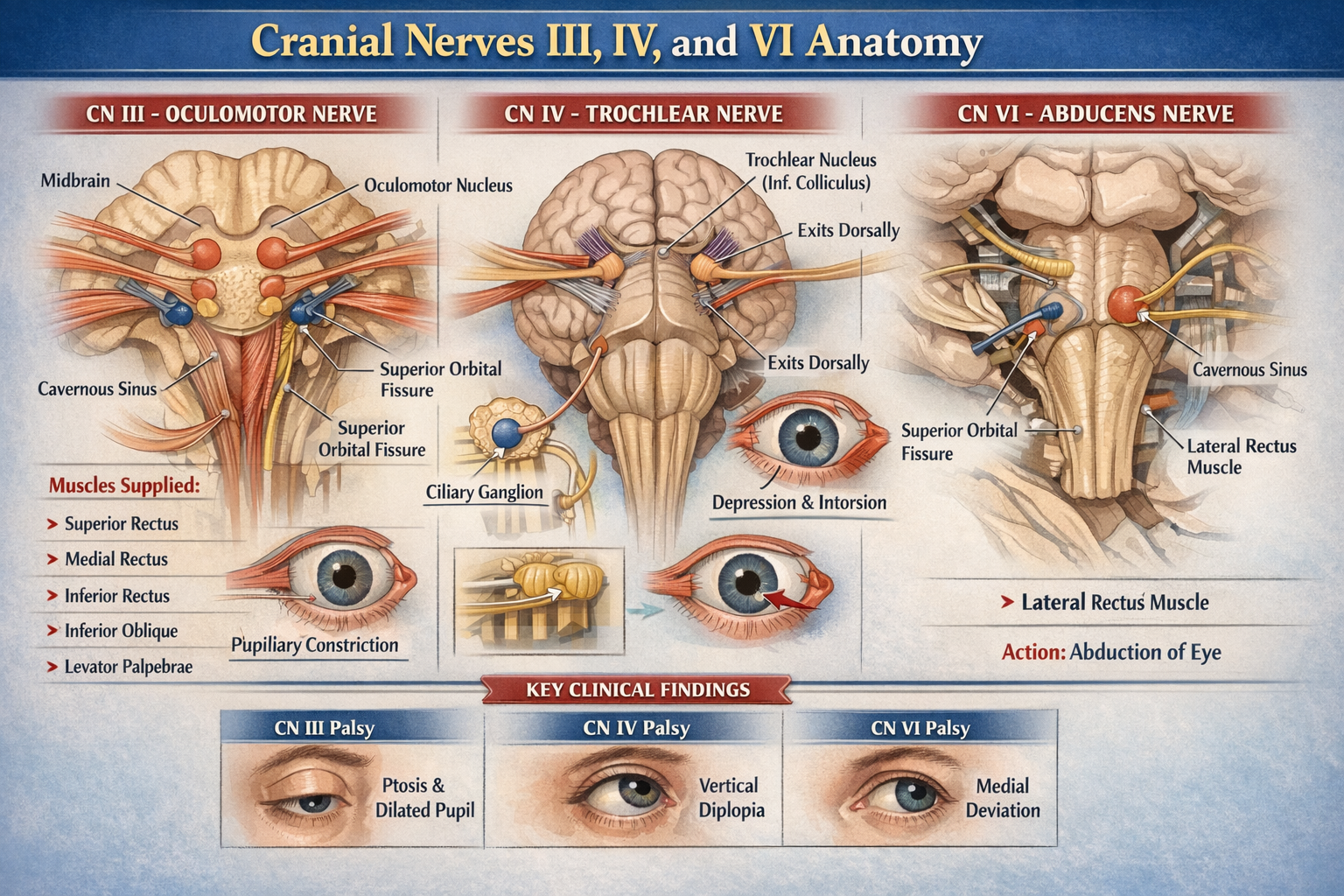
Cranial Nerves III IV VI Anatomy Detailed Overview for Medical Students
Frequently Asked Questions
Cranial nerves III IV and VI are motor cranial nerves responsible for controlling eye movements. They innervate the extraocular muscles that move the eyeball and maintain visual alignment.
The oculomotor nerve supplies most extraocular muscles, elevates the upper eyelid, constricts the pupil, and enables accommodation of the lens.
The oculomotor nuclear complex is located in the midbrain at the level of the superior colliculus.
Cranial nerve III supplies superior rectus, inferior rectus, medial rectus, inferior oblique, and levator palpebrae superioris muscles.
The trochlear nerve is the only cranial nerve that emerges from the dorsal surface of the brainstem, completely decussates, and has the longest intracranial course.
The trochlear nerve supplies the superior oblique muscle.
The superior oblique muscle causes intorsion and depression of the eyeball, especially when the eye is adducted.
The abducens nerve nucleus is located in the dorsal pons beneath the facial colliculus.
The abducens nerve innervates the lateral rectus muscle.
The lateral rectus muscle abducts the eyeball.
Cranial nerves III IV and VI pass through the cavernous sinus, with cranial nerve VI lying closest to the internal carotid artery.
All three nerves enter the orbit through the superior orbital fissure.
The abducens nerve has a long intracranial course and a sharp bend over the petrous apex, making it vulnerable to stretching in raised intracranial pressure.
Oculomotor nerve palsy causes ptosis, dilated pupil, loss of accommodation, and deviation of the eye downward and outward.
Trochlear nerve palsy typically presents with vertical diplopia that worsens when looking downwards, such as while descending stairs.
Abducens nerve palsy causes medial deviation of the eye due to unopposed action of the medial rectus muscle.
Parasympathetic fibers from the Edinger–Westphal nucleus travel with the oculomotor nerve to the ciliary ganglion.
The ciliary ganglion provides parasympathetic innervation to the sphincter pupillae and ciliary muscle.
The trochlear nerve enters the orbit outside the common tendinous ring.
These nerves are essential for coordinated eye movements, binocular vision, and pupillary reflexes, and their lesions cause characteristic diplopia and eye deviation patterns.
MCQ Test - Cranial Nerves III IV VI Anatomy Detailed Overview for Medical Students
No MCQs available for this article.